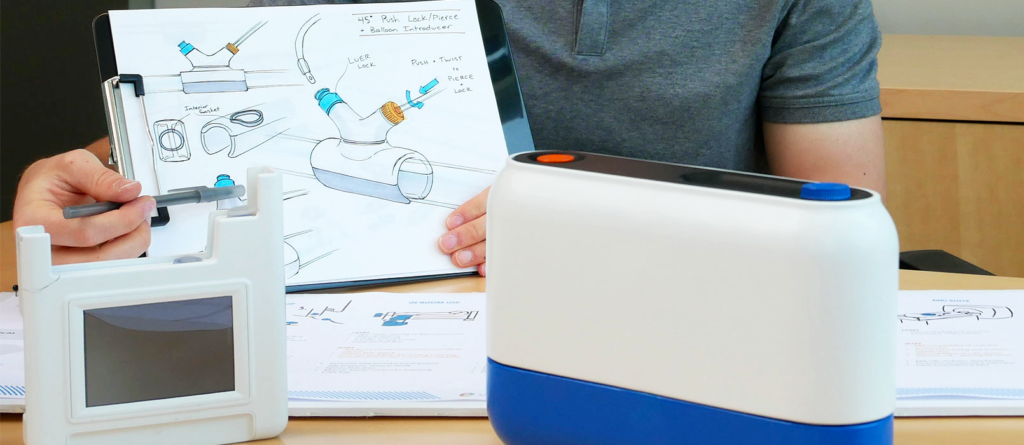
Nurse Error or Medical Device Design Problem
- Posted by Chris Justice
- On March 23, 2022
- Medical Device Design, Nurse Error, nurse faces prison
ABOUT THE AUTHOR(S)
Chris has accumulated many lessons-learned from 22 years of medical device design. Chris is principal and co-founder of Engenious Design, a medical device design firm that works with complex electro-mechanical & embedded software systems that are developed from scratch, acquired, and multi-generation products.